- Home Page
- Somerset Profile
- Local Community Network Profiles
- Electoral Division Profiles
- Joint Strategic Needs Assessment
- Census 2021
- Census 2011
- People & Neighbourhoods
- Health and Wellbeing
- Crime & Community Safety
- Economy & Jobs
- Education, Skills and Learning
- Environment
- Housing
- Travel and Access
- SINePost
- Children & Young People
- Older People
- Somerset Maps
- Somerset Geographies
- County Council Election Results
- Contact us
Pregnancy and Maternity

Public Health England profile
Health of babies, infants and young parents
Key priorities for Somerset
- Breastfeeding initiation needs to increase in areas where this remains low (primarily disadvantaged areas), and the drop-off rates from these areas prior to and during discharge from community midwifery to the health visiting service need to be reduced.
- Immunisations need to increase particularly in GP federation areas with the lowest uptake and for Children in Care.
- Smoking in pregnancy needs to be reduced through the identification and referral of pregnant women who smoke to stop smoking services and intensive support through dedicated smokefree families’ advisers.
- Vulnerable Young Parents require targeted support from the Health Visiting service working in partnership with midwifery services, social care and targeted youth services, building on the Young Parents Champion initiative.
- Maternity services to improve facilities across the county, and to lower the percentage of caesarean births
Low Birthweight
Low birth weight is defined as a weight under 2,500 grams. Many factors are associated with low birth weight including multiple pregnancy, maternal country of birth, poor maternal nutrition, lower socio-economic status and maternal smoking and drinking. Low birth weight is also associated with premature delivery.
- Somerset is better than the national average rate for low birth weight (<2500g) despite an increase of 0.6%, and in line with the norm for very low birth weight (<1500 grams)
- The proportion of all births which were of low weight has changed little in the past four years, at Somerset, South West region and England level.
|
|
< 1500 grams |
< 2500 grams |
||
|
2014 |
2015 |
2014 |
2015 |
|
|
England |
1.3 |
1.3 |
7.4 |
7.4 |
|
South West |
1.1 |
1.5 |
6.2 |
6.8 |
|
Somerset |
1.3 |
1.3 |
6.4 |
7.0 |
Source: National Child and Maternal Health Intelligence Network (released March 2017)
In the five-year period 2008-12, the Somerset wards with the highest proportion of low birth weight births (minimum at least 25 low birth weight births) were Street North (9.7%), Bridgwater Eastover (8.9%) and Shepton East (8.6%).
However, statistics on low birth rate have the potential to be misleading as babies may be delivered outside of the county due to neonatal intensive care facilities but are nonetheless resident in Somerset and likely to be learning / physically disabled.
For information on childhood immunisations see our Infectious Diseases page.
Perinatal Mortality
Perinatal mortality relates to still births and deaths in infants <7 days. The definition includes foetal deaths occurring after 24 weeks of gestation. The perinatal mortality rates tend to be higher than infant mortality rates because many babies born with very serious health problems may be born live but are unable to survive beyond a few days.
- There were 111 stilbirths or deaths within 7 days in Somerset for 2011-13.
- The perinatal mortality rate in Somerset for 2011-13 is 6.5 per 1000 total births, not significantly different from the regional and national rates of 6.4 per 1000 and 7.1 per 1000 births, respectively.
- This latest figure for Somerset is an improvement on the 2009-11 peak of 7.5 per 1000 births, but in line with the levels seen several years ago (see chart below). (Source: CHIMAT)
Trends in Perinatal Mortality rate (rolling 3-year periods) 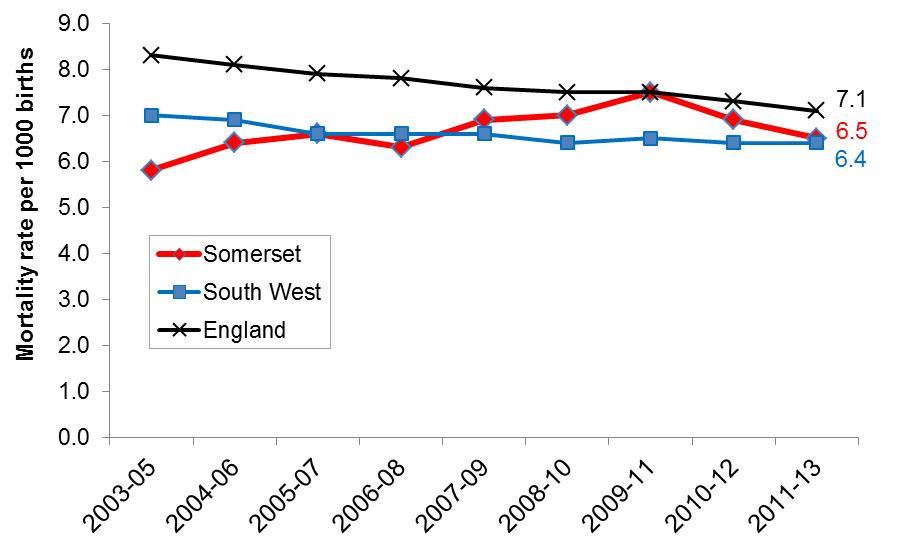
Source: ChiMat
Infant Mortality
Traditionally, infant and childhood mortality has been seen as a major indicator of the health of a nation. During the 20th century, infant and childhood mortality rates in England dropped significantly in response to a variety of factors and interventions that include improved living conditions, diet and sanitation, birth control, advancements in medical science and the availability of health care. Despite this, inequalities have not reduced and important differentials exist by father’s social class, birth weight, mother’s country of birth, marital status of parents, sex and multiple birth status. It is also known that one of the major determinants of infant mortality is social deprivation. Low income groups have higher rates of children born with low birth weight and infant mortality compared with higher income groups.
Infant mortality measures the probability of dying in the time between birth and exactly one year of age. As rates have declined, the proportion of cases that can be influenced by better maternal health or health care interventions also decreases.
- There were 68 deaths in infants under one year in Somerset in the 2011-13 period.
- Somerset’s infant mortality rate is in line with both regional and national averages (see below)
Trends in Infant Mortality rate (rolling 3-year periods) 
Source: ChiMat
For more data on child and infant mortality, please see the National Child and Maternal Health Intelligence Network
Programmes in Somerset to improve pregnancy and maternity health
There are a number of programmes in Somerset to improve health during pregnancy and into early infancy. In particular, priorities include:-
- reducing smoking in pregnancy
- lower percentage of caesareans, (with a higher percentage having vaginal birth after caesarean, VBAC)
- higher percentage of women breastfeeding at birth, discharge, 3 months and 6 months
- a reduction in teenage pregnancies and improved support for teenage parents
- improvement of maternity facilities across the county.
Somerset Partnership NHS Foundation Trust have developed and rolled out the Pregnancy, Birth and Beyond (PBB) initiative. Staff will review the current Antenatal and Postnatal group structure and content to impact assess the PBB programme and where necessary update to meet the PBB standards, and this will be audited next year. They also undertook a survey of the health needs of Central and Eastern European migrant families in South Somerset and identified amongst other issues the need for better links by health visitors with GPs to improve the uptake of immunisations in this group.
Some of the main programmes to improve maternal health are detailed below.
Breastfeeding
To improve health and reduce inequality by increasing the initiation and prevalence of breastfeeding amongst the Somerset population; particularly targeting the most vulnerable groups.
It is well recognised that there are differences in the determinants of health between different groups of people so the breastfeeding and infant nutrition strategy aims to reduce the gap and improve the health outcomes of babies and their mothers across the population.
Improvements in breastfeeding are measured by initiation rates (number of babies who commence breastfeeding regardless of how long), and prevalence rates (the number of babies who are totally and partially breastfed at the 6-8 week check.
Breastfeeding initiation and prevalence is lowest amongst mothers from disadvantaged groups. Young mothers under 24 years and teenage parents are less likely to breastfeed or discontinue breastfeeding soon after initiation. Breastfeeding initiation is found to be significantly associated with deprivation.
Breastfeeding prevalence increases with maternal age and decreases with greater deprivation. (Somerset Breastfeeding Health Equity Audit)
Evidence has shown that babies who are breast-fed are less likely to suffer from, or be hospitalised for, gastro-intestinal or respiratory infections. There is also increasing evidence that breastfeeding in the early months of life can reduce the risk of obesity in later life. In addition to the benefits for the child breastfeeding also reduces the risk of breast and ovarian cancer for the mother.
Key facts for Somerset
-
The August 2015 Public Health Outcomes Framework shows the initiation rates for Somerset were 82.6 % while the total for the South West was 78.6%. Both of these figures were above the national average which was 73.9 %.
-
The Prevalence (at the 6-8 week check) for Somerset was 48.5%, while the Southwest South West 49.3%. (Due to incomplete data England prevalence data was unable to be published). See table below.
|
|
Breastfeeding Initiation |
Breastfeeding at 6-8 weeks |
|
England |
73.9% |
|
|
South West |
78.6% |
49.3% |
|
Somerset |
82.6% |
48.5% |
Source: August 2015 Public Health Outcomes Framework
-
Breastfeeding initiation was lowest in under 24 year olds (<71%) and increased significantly in over 29 year olds (>89%)
-
Breastfeeding initiation was lowest in Sedgemoor district (79%)
- Breastfeeding initiation was highest in Taunton Deane and West Somerset (84%)
Current Service Provision
Somerset is served by two main acute trusts that provide maternity services (Taunton and Somerset NHS Foundation Trust and Yeovil District Hospital NHS Foundation Trust). The sole provider of Health Visiting services in Somerset is Somerset Partnership NHS Trust.
The UNICEF Baby Friendly Initiative (BFI) provides a framework for the implementation of best practice in breastfeeding.
All three main providers of Midwifery and Health Visiting services are World Health Organisation (WHO) ‘Baby Friendly Initiative’ accredited. All three attend an established Breastfeeding and Infant Nutrition Steering group along with representatives from Somerset County Council Public Health Team.
Somerset County Council is currently in the process of rolling out ‘Breastfeeding Welcome’, a programme whereby local businesses agree to specified criteria that support and enable breastfeeding in their establishment.
Somerset Partnership NHS Foundation Trust have established breastfeeding support groups throughout the county and are available for attendance weekly. These are particularly concentrated in areas of high need i.e. greatest proportion of LSOA’s in Somerset.
Somerset has a breastfeeding peer support programme. Breastfeeding mothers can speak to their health visitor about joining this programme.
Future Needs of the Population
The aim is to increase and sustain the high initiation rates and to decrease the drop-off rate between initiation and 6-8 weeks.
Somerset County Council Public Health is updating the Breastfeeding and Infant Nutrition Strategy, due for completion April 2016. The strategy will target initiatives at the groups identified in the Health Equity Audit (April 2014- March 2014).
Recommendations for Action:
- Publication and implementation of the breastfeeding and Infant Nutrition Strategy
- Organisations and services with BFI to continue to achieve reaccreditation
- Public Health Intelligence are completing a ‘snapshot’ analysis of breastfeeding prevalence up to and including the 6-8 week check. The findings will be used to inform the strategy.
References and further reading:
Somerset County Council Breastfeeding Health Equity Audit (April 2013 - March 2014)
Somerset Breastfeeding and Infant Nutrition Strategy (due for completion 2016)
Young Parents
Evidence shows that young mothers and their babies experience poorer health outcomes in comparison to general maternal health. Young mothers are more likely to smoke during pregnancy, less likely to breastfeed and more likely to have post natal depression. This is often compounded by the fact that many young parents come from the most deprived areas.
Following concerns about the lack of a joined up multi agency approach in the service provision for vulnerable young parents within Somerset, it was agreed that a model of targeted service delivery would be developed. It was identified that there was a need to set up a service within the Health Visiting service to meet the needs of vulnerable young pregnant/parents including care leavers.
Following a pilot and research into other models themes were identified that informed the development of this work with young parents in Somerset, as well as future training needs of staff. These were:
- early ante-natal relationship building
- adapted styles of communication
- a focus on the promotion of attachment
- engagement of young fathers
Somerset Partnership NHS Foundation Trust have led on the development of an Antenatal Workbook to use as part of a structured approach to working with young parents. A Postnatal Workbook, a website and smartphone App are also in development.
During January and February 2013 13 Young Parent Champions were recruited from the Health Visiting team, with the aim to have at least one Champion per GP Federation Team. In February 2013 the Young Parent Champions commenced recruiting young parents to the service and began to pilot the Antenatal Workbook. Since February 2013 a total of 196 Young Parents have been recruited to the programme. The age range of young parents engaged in the service is between 14 to 21years old, with the majority between 16 and 19 years old.
A monthly clinical supervision session commenced as part of the Young Parents Champion Meeting to provide an opportunity to discuss areas of concern and common themes experienced when working with this vulnerable client group. This has highlighted that a number of the young parents engaged in the programme have had previous/continued involvement with CAMHS and/or Children’s Social Care. Access to appropriate housing and benefits is also a common feature, which again emphasises the increased intervention required when supporting this client group. Additional specialist mental health clinical supervision for Health Visitors is being explored as a consequence of this. The complexity of the families has also indicated the need for all young parents on the caseloads to be highlighted and discussed at Child Protection supervision.
The following actions are recommended to support the work of the Young Parent Champions:-
- continued discussions with commissioners on how the Health Visiting service can be supported to deliver this enhanced provision to this vulnerable client group.
- all Young Parents on the Health Visitor caseload should be highlighted and discussed at child protection clinical supervision
- Mental health supervision should be commenced with the Young Parent Champions
- the Young Parent Programme Lead should deliver presentations to each of the area teams to highlight the need for supporting this area of work and offering targeted work with this client group as a priority.
- training should be rolled out to all teams on working with Young Parents, highlighting the risk factors associated with this client group and the impact this has on outcomes.
Further information:
- For more data, see Somerset Child Health Profile 2016
- Smoking in pregnancy - see our Smoking and Tobacco Control page.
To return to the top of the page, please click here
 Read our SINePost monthly newsletter
Read our SINePost monthly newsletter
Did you know?
The proportion of Christians in Somerset declined from 76.7% in 2001 to 64.0% in 2011. The proportion of people who said they had no religious affiliation increased from 14.8% to 26.6% over the same period. - 2011 Census